Search News Archives
Filter News Articles
Additional Navigation
Engineering professor contributes to research on containment of COVID-19 in hospitals nationwide
March 31, 2020 : By Jacob Couch - Office of Communications & Public Engagement
Liberty University Professor of Mechanical Engineering Dr. Wayne Strasser was recently asked by Vapotherm, a company focused on the development of respiratory therapy products, to aid them in their research on the spread of COVID-19.
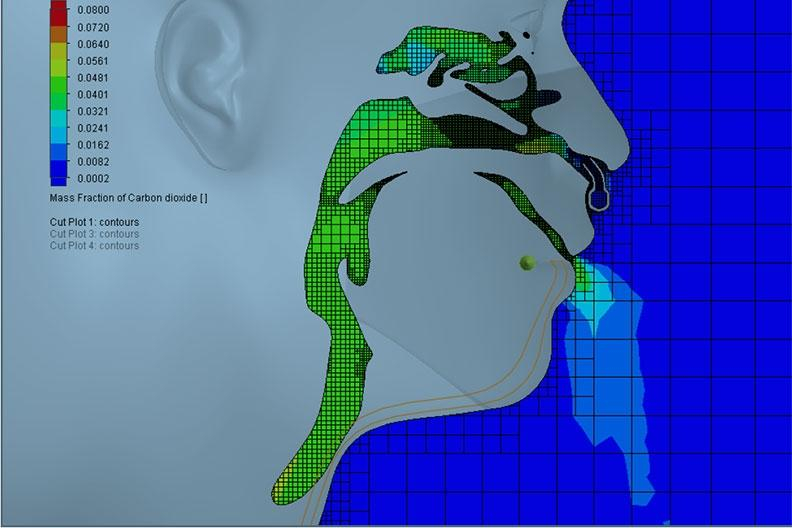
 Strasser has been constructing computer models (using Computational Fluid Dynamics) of infected hospital patients receiving therapy in order to assist Vapotherm in testing their patented high-velocity respiratory therapy equipment. The goal is to make sure the equipment isn’t quickening the spread of COVID-19 from patients receiving treatment for the virus.
Strasser has been constructing computer models (using Computational Fluid Dynamics) of infected hospital patients receiving therapy in order to assist Vapotherm in testing their patented high-velocity respiratory therapy equipment. The goal is to make sure the equipment isn’t quickening the spread of COVID-19 from patients receiving treatment for the virus.
“Vapotherm contacted Liberty first, before any other institution, to work on these computer models,” Strasser said. “The Centers for Disease Control and Prevention (CDC) has asked them for data assessing whether or not their high-velocity therapy somehow exacerbates the spread of the virus for patients in the hospital who are already tagged with the virus and are receiving that respiratory therapy with the high-velocity nasal cannula.” (A nasal cannula is a tube placed in the nostrils that delivers oxygen and increases airflow).
Strasser’s work focused on running computer simulations that mimic patients receiving varying levels of therapy. The computer models show, in real-time, how the patient’s breathing patterns and the position of a mask on the patient affect the potential for the spread of infectious diseases.
“My job was to build a replica of a patient in a bed in a hospital room with typical ventilation and build that in computational space, such that it’s a computer model that is a replica, or mimic, of a patient lying on a table receiving this respiratory therapy,” Strasser said. “Assuming the patient has tested positive, and evaluating the level of respiratory therapy we are giving the patient, we study the spread of airborne mucus particles from the patient’s nose and throat and where those particles land in the room … whether it lands on the patient or is captured in the mask she is wearing and how those differentiate as they spread around the room.”
Strasser and Ph.D. student Reid Prichard have discerned that the preliminary results indicate the therapy is not as bad as the CDC feared. The results shows that a patient’s mask significantly mediates the risk.
“We’re not saying that the mask will completely solve the problem, but we do know that the mask, by far, captures most of the particles,” Strasser said. “My computer models test how the level of therapy affected those particles.”
Strasser said that although there is leakage of infected saliva and mucus particles around the mask, the majority of particles are filtered.
“We are now doing a second look at the same six models with a more robust and refined numerical approach such that we can more accurately capture the spread of different-sized groups of particles,” Strasser said.
Strasser pointed out that germs on their own are too small for masks to capture, but the primary concerns are the large groups of saliva and mucus particles that we emit when we cough, sneeze, or breathe. He said that masks often catch these particles.
Strasser and Prichard will attempt to experiment with designing masks that are more comfortable and cooler for patients to wear.
“We are probably going to try some things related to cooling therapy, so that the patients don’t feel warm around their face with mask restrictiveness,” Strasser said.
Strasser holds bachelor’s and master’s degrees from Clemson University as well as a Ph.D. from Virginia Tech. He specializes in the areas of turbulence, unsteadiness, industrial equipment, and multiphase reactors.
He said he is grateful that he has the privilege of playing a part in attempting to lessen the spread of COVID-19.
“I praise the LORD for these opportunities.”


